Brazil Dentists Digital Transformation Training Pain Points: The Real Learning Curve from Traditional to CAD/CAM in 2026
2026-01-08
2025-12-17
In South Africa's evolving healthcare landscape, Computer-Aided Design (CAD) and Computer-Aided Manufacturing (CAM) systems represent a transformative technology, particularly in dental care. These systems enable precise design and fabrication of dental prosthetics like crowns, bridges, and implants, often in a single visit. For small clinics, which dominate the private sector—accounting for over 70% of dental practices according to the South African Dental Association (SADA) data from 2024—adopting cost-effective CAD/CAM could enhance efficiency, reduce patient wait times, and improve outcomes.
However, the path to integration is fraught with challenges. South Africa's healthcare system grapples with resource disparities, with rural and township clinics facing amplified barriers. A 2023 report by the World Health Organization (WHO) indicates that only 15-20% of dental facilities in sub-Saharan Africa, including South Africa, have adopted advanced digital technologies. This article delves into the primary obstacles for small clinics in adopting cost-effective CAD/CAM systems, drawing on data from sources like the African Development Bank (AfDB), United Nations Industrial Development Organization (UNIDO), and local health studies. By addressing these, clinics can move toward sustainable digital adoption, potentially boosting service delivery in a country where dentist-to-population ratios stand at 1:4,000, per 2024 Health Professions Council of South Africa (HPCSA) figures.

One of the most significant hurdles is the financial burden associated with CAD/CAM implementation. Cost-effective systems, designed to minimize expenses through modular setups and open-source software, still require substantial upfront investments. According to a 2025 UNIDO analysis, the average cost for basic CAD/CAM hardware and software in African markets ranges from $20,000 to $50,000, excluding installation and training. For small clinics in South Africa, where annual revenues often fall below $100,000 as per a 2024 AfDB survey of SMEs in healthcare, this represents 20-50% of yearly income, making it prohibitive.
Maintenance and operational costs further exacerbate the issue. Recurring expenses for software updates, calibration, and materials can add 10-15% annually to the initial outlay, based on a 2023 study in the Journal of Health Workforce and Capacity Research. In regions like Gauteng and KwaZulu-Natal, where electricity tariffs have risen by 12% in 2025 per Eskom reports, energy-intensive CAD/CAM machines increase utility bills by up to 25%. Currency fluctuations, with the Rand depreciating 8% against the USD in 2025 (Reserve Bank data), inflate import costs since over 80% of components are sourced internationally, as noted in a 2024 WTO trade review.
Small clinics often lack access to financing. Government subsidies under the National Health Insurance (NHI) framework, piloted since 2012, cover only basic equipment, excluding advanced tech like CAD/CAM. A 2025 Brookings Institution report highlights that fewer than 10% of small healthcare providers secure loans for digital upgrades due to high interest rates averaging 15-20% from local banks.
South Africa's infrastructure deficits pose another layer of complexity. Reliable electricity is crucial for CAD/CAM operations, yet load-shedding affects 60% of clinics, per a 2024 WHO infrastructure assessment. In rural areas like Limpopo and Eastern Cape, power outages average 4-6 hours daily, disrupting scanning and milling processes that require uninterrupted power. Backup generators, while a solution, add costs of $5,000-$10,000 initially, plus fuel expenses, deterring adoption.
Internet connectivity is equally vital for cloud-based CAD/CAM features, such as remote design collaboration. However, broadband penetration in South Africa stands at 45% in urban areas and drops to 20% in rural zones, according to 2025 ICASA (Independent Communications Authority of South Africa) statistics. Slow speeds—averaging 25 Mbps nationally—lead to data transfer delays, increasing procedure times by 30-50%, as evidenced in a 2023 Frontiers in Digital Health study on EHR implementation barriers.
Physical space constraints in small clinics compound these issues. Many operate in limited facilities under 200 square meters, per a 2024 HPCSA clinic survey, leaving insufficient room for CAD/CAM equipment like scanners and mills. Urban-rural divides amplify this; township clinics in Johannesburg face zoning restrictions, while remote ones lack transport links for equipment delivery, with logistics costs inflating by 40% in remote areas (AfDB 2024 logistics index).
Skill gaps represent a critical barrier. CAD/CAM adoption demands proficient users, yet South Africa faces a dentist shortage, with only 6,000 registered practitioners for 60 million people (HPCSA 2024). Training programs are scarce; a 2025 study in BMC Medical Education notes that fewer than 25% of dental curricula at universities like Witwatersrand and Pretoria include hands-on CAD/CAM modules.
For small clinics, staff training costs $2,000-$5,000 per person, including travel to urban centers, per SADA estimates. Post-training support is limited, leading to underutilization; a 2023 ResearchGate publication on dental records in South Africa found that 40% of trained users revert to manual methods due to inadequate follow-up. Nurses and assistants, who handle much of the workflow in small setups, often lack digital literacy, with adoption rates below 30% in public clinics (NIH 2025 study on EHR adoption by nurses).
Cultural resistance adds to this. Older practitioners, comprising 50% of the workforce (HPCSA demographics), prefer traditional methods, viewing CAD/CAM as complex. A 2024 survey in the Journal of Health Workforce and Capacity Research revealed that 35% of dentists cite "fear of technology failure" as a deterrent.
Navigating regulations slows adoption. South Africa's Medicines and Related Substances Act requires CAD/CAM-produced prosthetics to meet stringent standards, but certification processes take 6-12 months, per 2025 SAHPRA (South African Health Products Regulatory Authority) guidelines. Small clinics struggle with compliance documentation, facing fines up to $10,000 for non-adherence.
Policy inconsistencies hinder progress. While the Digital Health Strategy 2019-2024 promotes tech adoption, implementation lags; a 2025 Frontiers in Digital Health article identifies weak governance as a key barrier, with only 15% of clinics receiving NHI tech grants. Data privacy under POPIA (Protection of Personal Information Act) adds complexity, requiring secure systems that increase costs by 10-20%.
Intra-African trade under AfCFTA could alleviate import duties, but bureaucratic delays mean benefits are unrealized for small players, with tariffs still at 10-15% on tech imports (WTO 2024).
Examining specific cases illustrates these challenges.
In Cape Town, a small township clinic attempted CAD/CAM adoption in 2023. Initial costs exceeded budget by 25%, leading to partial implementation. Power issues caused 20% downtime, reducing patient throughput (case from 2025 Yucera blog on innovations, anonymized).
A rural Limpopo clinic, per a 2024 UNIDO report, abandoned plans due to training shortages; only one staff member completed certification, insufficient for operations.
In contrast, an urban Durban clinic overcame barriers through partnerships, securing a grant that cut costs by 30%, but this is rare—only 5% of small clinics access such aid (AfDB 2025).
These examples underscore that while benefits like 30% cost reductions in treatments (2025 Yucera analysis) are possible, systemic issues prevail.
Adoption challenges perpetuate inequalities. In underserved areas, where 70% of the population relies on public or small private clinics (Stats SA 2024), delayed tech integration means prolonged wait times—up to 4 weeks for prosthetics versus same-day with CAD/CAM.
Economically, unaddressed barriers cost the sector $500 million annually in lost productivity (WHO 2025 estimate for Africa, prorated for South Africa). Socially, it affects women and youth, who form 60% of dental patients in low-income brackets (HPCSA 2024).
Environmentally, inefficient manual processes generate more waste; CAD/CAM could reduce material use by 25%, per IEA 2024 reports, but adoption lags hinder this.
To mitigate these, targeted strategies are essential. Governments could expand subsidies; the NHI could allocate 10% of its $20 billion budget (2025 Treasury figures) to tech grants. Public-private partnerships, like those in the Digital Economy for Africa initiative, aim to train 50,000 health workers by 2030 (World Bank 2025).
Clinics can opt for phased adoption, starting with software-only modules costing under $5,000. Collaborations with universities for on-site training could address skills gaps.
Looking ahead, emerging AI integrations could lower costs by 20-30% (2025 Yucera insights), making CAD/CAM more accessible. By 2030, adoption could rise to 40% if barriers are addressed, per UNIDO projections, fostering resilient healthcare.
In conclusion, while cost-effective CAD/CAM systems offer promise for South African small clinics, financial, infrastructural, human, and regulatory challenges impede progress. Strategic interventions can transform these obstacles, enhancing dental care equity and efficiency across the nation.

Dry & wet milling for zirconia, PMMA, wax with auto tool changer.
learn more
High-precision 3D scanning, AI calibration, full-arch accuracy.
learn more
40-min full sintering with 57% incisal translucency and 1050 MPa strength.
learn more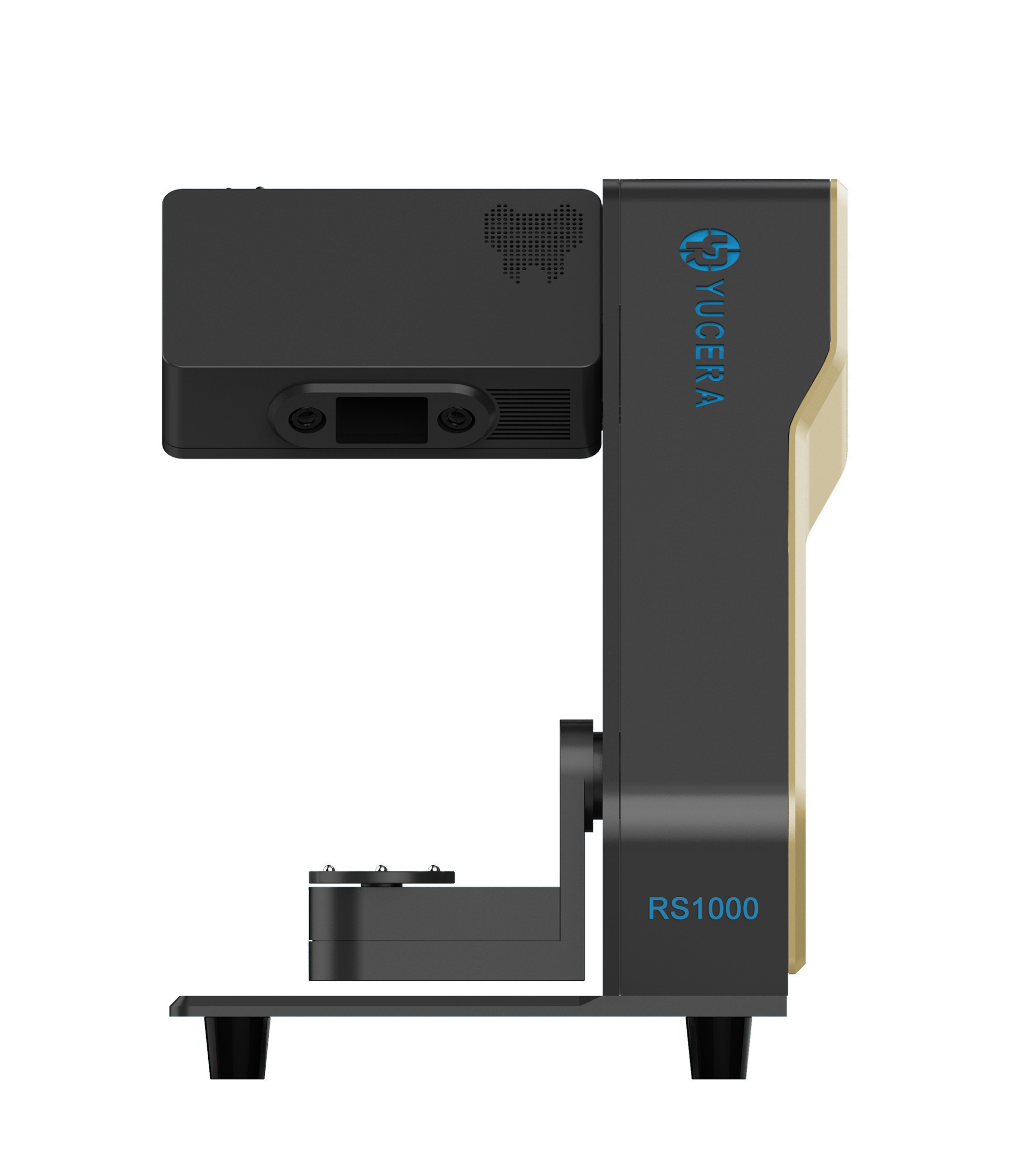

40-min cycle for 60 crowns, dual-layer crucible and 200°C/min heating.
learn more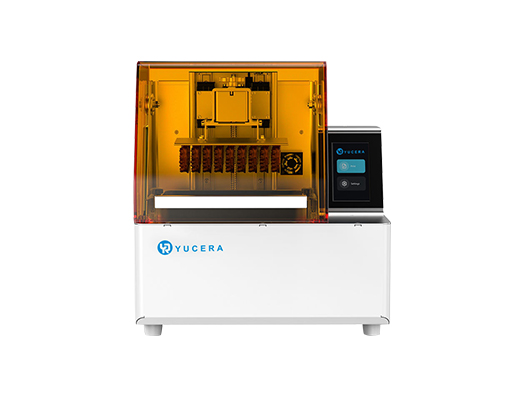
High-speed LCD printer for guides, temporaries, models with 8K resolution.
learn more